Diabet Step‑by‑Step Guide to Balanced Daily Habits: Achieving a Healthier You
Navigating the complexities of diabetes management can feel overwhelming. The constant monitoring, dietary adjustments, and medication schedules demand significant effort. This comprehensive guide, a Diabet Step‑by‑Step Guide to Balanced Daily Habits, provides a practical roadmap. It empowers individuals to take control of their health and live fulfilling lives. This article offers actionable steps. It focuses on building sustainable, balanced daily habits. These habits are crucial for effective diabetes management.
Understanding the Foundation: Diabetes and Its Impact
Diabetes, a chronic metabolic disorder, affects millions worldwide. It is characterized by elevated blood sugar levels. This occurs due to the body’s inability to produce or effectively use insulin. Insulin, a hormone produced by the pancreas, is essential for glucose uptake. Glucose is the primary energy source for cells. There are several types of diabetes. Type 1 diabetes is an autoimmune condition. The body attacks and destroys insulin-producing cells. Type 2 diabetes is the most common form. It develops when the body becomes resistant to insulin. Or, the pancreas gradually loses its ability to produce it. Gestational diabetes occurs during pregnancy. It often resolves after childbirth. Regardless of the type, understanding the impact of diabetes is critical. Untreated diabetes can lead to serious complications. These complications include cardiovascular disease, nerve damage, kidney disease, and vision loss. Therefore, a proactive approach to diabetes management is paramount.
Step One: Prioritizing Blood Sugar Monitoring
Regular blood sugar monitoring is the cornerstone of effective diabetes management. It provides real-time feedback on how lifestyle choices affect blood glucose levels. This information is invaluable for making informed decisions. It helps in adjusting medication dosages and dietary plans. The frequency of blood sugar monitoring varies. It depends on the individual’s diabetes type, treatment plan, and overall health. People using insulin often need to check their blood sugar several times a day. This includes before meals, before bedtime, and sometimes after meals. Those managing diabetes with diet and oral medications may need less frequent monitoring. A healthcare professional will provide personalized guidance. They determine the appropriate monitoring schedule. Blood glucose meters are readily available. They are relatively easy to use. They provide quick and accurate results. Continuous glucose monitors (CGMs) are also an option. They offer continuous blood sugar readings. They provide valuable insights into glucose trends. They also offer alerts for high or low blood sugar levels. Keeping a log of blood sugar readings is essential. This log should include the time of day, blood sugar level, and any relevant details. This includes food consumed and medications taken. This log is crucial for tracking progress and identifying patterns. It also helps in communicating effectively with healthcare providers.
Step Two: Mastering the Art of Dietary Management
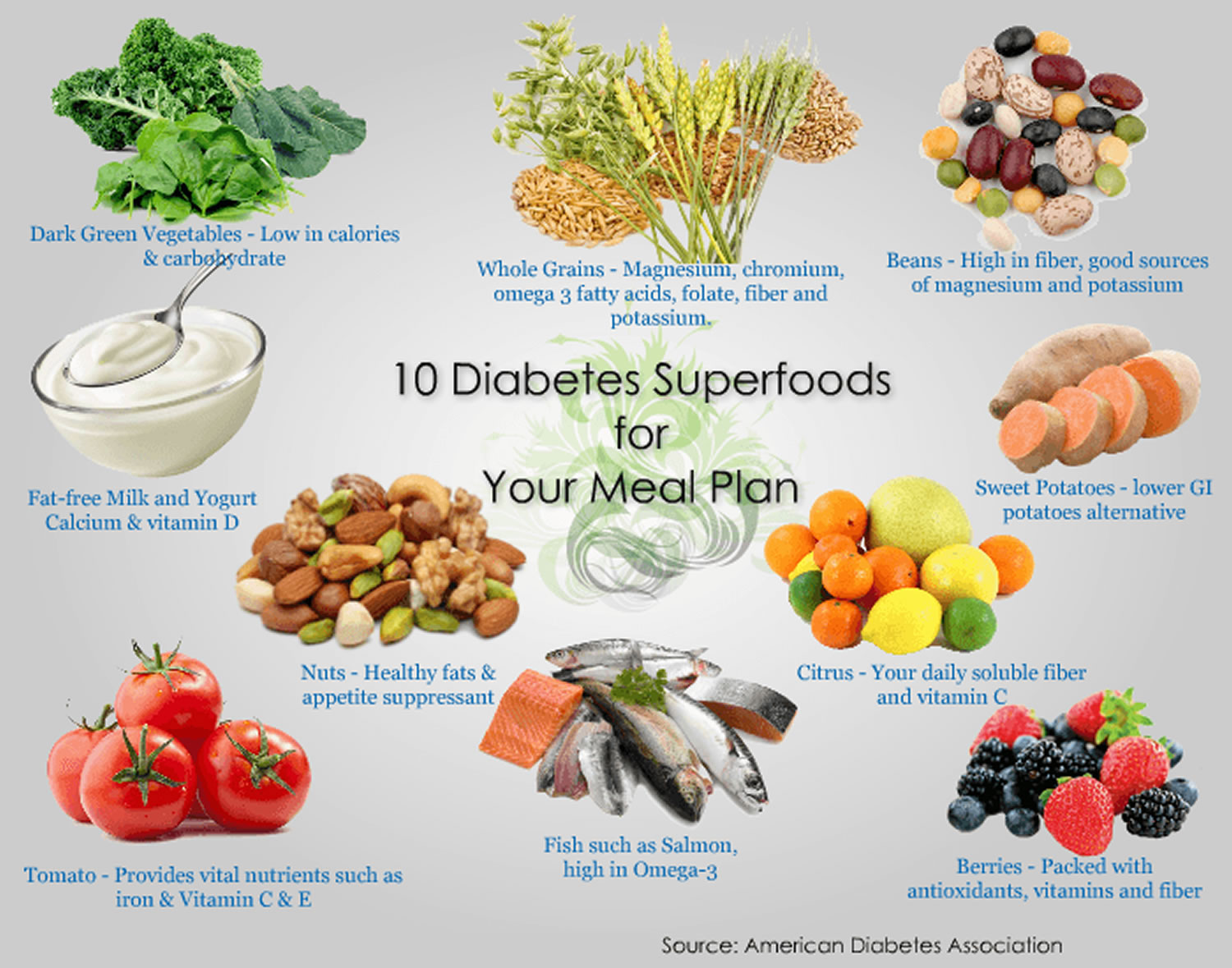
Diet plays a central role in diabetes management. A well-planned diet helps regulate blood sugar levels. It supports overall health and reduces the risk of complications. The principles of a diabetes-friendly diet are similar to those of a healthy diet for anyone. It emphasizes whole, unprocessed foods. It also focuses on portion control. It includes a balanced intake of carbohydrates, proteins, and fats. Carbohydrates have the most significant impact on blood sugar levels. It is important to choose carbohydrate sources wisely. Focus on complex carbohydrates like whole grains, fruits, vegetables, and legumes. These foods are digested more slowly than refined carbohydrates. They cause a gradual rise in blood sugar. Limit the intake of sugary drinks, processed foods, and refined grains. These foods can cause rapid blood sugar spikes. Protein helps slow down the absorption of carbohydrates. It promotes satiety. Include lean protein sources in every meal. These include fish, poultry, beans, and tofu. Healthy fats are also essential. They support overall health and reduce the risk of heart disease. Choose unsaturated fats like those found in avocados, nuts, and olive oil. Limit saturated and trans fats. Portion control is critical for managing blood sugar levels. Use smaller plates. Measure food portions. Pay attention to hunger and fullness cues. Work with a registered dietitian or certified diabetes educator. They can develop a personalized meal plan. This plan considers individual needs and preferences. This plan will also provide guidance on carbohydrate counting. They will also provide support for making sustainable dietary changes.
Step Three: Embracing Regular Physical Activity
Physical activity is a powerful tool for managing diabetes. It improves insulin sensitivity. It helps the body use glucose more effectively. Regular exercise also promotes weight loss. It reduces the risk of cardiovascular disease. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week. This includes brisk walking, cycling, or swimming. Include strength training exercises at least two days a week. Strength training helps build muscle mass. Muscle mass improves insulin sensitivity. Choose activities you enjoy. This will make it easier to stick with an exercise routine. Consult with a healthcare provider before starting a new exercise program. They can provide recommendations based on your individual health needs. Monitor blood sugar levels before, during, and after exercise. This is essential to understand how exercise affects your blood glucose. Adjust medication or carbohydrate intake as needed. Stay hydrated by drinking plenty of water before, during, and after exercise. This is crucial for preventing dehydration.
Step Four: Adopting Stress Management Techniques
Stress can significantly impact blood sugar levels. It triggers the release of stress hormones. These hormones can raise blood glucose. Chronic stress can make diabetes management more challenging. It can also increase the risk of complications. Incorporate stress management techniques into your daily routine. These include deep breathing exercises, meditation, and yoga. Engage in activities you find relaxing. This includes spending time in nature, listening to music, or pursuing hobbies. Prioritize sleep. Aim for seven to nine hours of quality sleep per night. Sleep deprivation can worsen insulin resistance and increase stress levels. Build a strong support system. Connect with friends, family, or a support group. Seek professional help if needed. A therapist or counselor can provide guidance and support. They can also help you develop effective coping strategies for managing stress.
Step Five: Prioritizing Regular Medical Checkups
Regular medical checkups are essential for comprehensive diabetes management. These checkups help monitor overall health. They also help prevent and manage complications. See your healthcare provider at least twice a year. This will include a physical exam, blood tests, and a review of your medication. Undergo an annual eye exam. Diabetes can damage blood vessels in the eyes. Early detection and treatment are crucial for preventing vision loss. Schedule regular foot exams. Diabetes can cause nerve damage and poor circulation in the feet. This can lead to foot ulcers and infections. Get vaccinated against the flu and pneumonia. People with diabetes are at higher risk for these infections. Work closely with your healthcare team. This includes your primary care physician, endocrinologist, registered dietitian, and certified diabetes educator. Ask questions. Discuss any concerns you have. Follow your healthcare provider’s recommendations. This is essential for maintaining optimal health.
Step Six: Understanding and Managing Medications
Medications play a crucial role in managing diabetes. They help regulate blood sugar levels. They also reduce the risk of complications. There are various types of diabetes medications. Each works differently to lower blood glucose. Oral medications include metformin, sulfonylureas, and others. Insulin is a medication administered by injection or an insulin pump. Work with your healthcare provider to determine the appropriate medication regimen. Understand how your medications work. Learn about potential side effects. Take your medications as prescribed. Never change your dosage or stop taking your medications without consulting your healthcare provider. Keep a record of your medications. This includes the name, dosage, and time of administration. This will help ensure you take your medications correctly. Store your medications properly. Follow the storage instructions provided by your pharmacist. Regularly review your medications with your healthcare provider. This will help ensure they are still appropriate and effective.
Step Seven: Building a Supportive Environment
Creating a supportive environment is crucial for successful diabetes management. This includes both physical and emotional support. Communicate your needs to your family and friends. Educate them about diabetes. Encourage them to support your healthy lifestyle choices. Join a diabetes support group. Connect with other people living with diabetes. Share experiences, and offer mutual encouragement. Seek support from healthcare professionals. This includes your doctor, dietitian, and certified diabetes educator. Create a diabetes-friendly home environment. This includes having healthy food options readily available. Keep exercise equipment accessible. Make sure your home is safe and accessible. Celebrate your successes. Acknowledge your progress. Reward yourself for achieving your goals. Be kind to yourself. Diabetes management is an ongoing process. There will be ups and downs. Learn from setbacks. Keep moving forward. Remember that you are not alone. Many resources are available to help you succeed.
Conclusion: Embracing a Healthier Future
The Diabet Step‑by‑Step Guide to Balanced Daily Habits offers a comprehensive framework. It supports individuals in managing their diabetes effectively. By prioritizing blood sugar monitoring, dietary management, physical activity, stress management, regular medical checkups, medication management, and building a supportive environment, individuals can take control of their health. They can also reduce the risk of complications. They can live fulfilling lives. Remember that consistency and persistence are key. Make small, sustainable changes. Celebrate your progress. Embrace a healthier future. This detailed Diabet Step‑by‑Step Guide to Balanced Daily Habits equips you with the knowledge. It empowers you to make informed decisions. It is about achieving a healthier and more fulfilling life. This journey requires dedication. It offers the ultimate reward: improved health and well-being.
[See also: Related Article Titles]